Benjamin Mateus
A second individual, known as the “London patient,” has been recently confirmed to be free of the human immunodeficiency virus (HIV) infection after receiving a bone marrow transplant for Hodgkin’s lymphoma from a donor with a genetic resistance to the virus. Thirty months after the transplant, multiple tests indicate there is “no return of the virus.”
At this stage, the virus is considered to be in remission. Specialists in the field suggest a three- to four-year period to confidently confirm the cure.
A possible third case was recently announced on March 6 at a conference on retroviruses and opportunistic infections held in Seattle. The “Dusseldorf patient” has shown no signs of infectious HIV more than three months after discontinuing antiviral medications. There are six other HIV-infected patients who have received bone marrow transplants from donors resistant to the virus and might in the future be deemed cured.
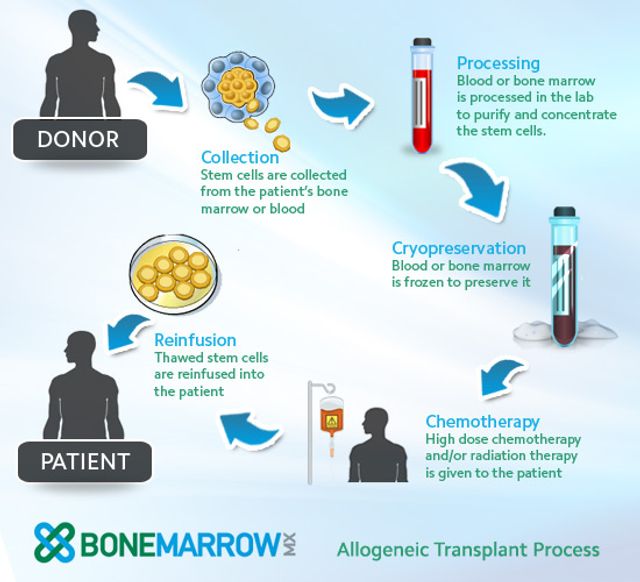 Diagram of the bone marrow transplant process. Credit: BONEMARROWmx
Diagram of the bone marrow transplant process. Credit: BONEMARROWmx
HIV is a sexually transmitted virus and the precursor to acquired immunodeficiency syndrome (AIDS), one of the most widespread and deadly diseases on the planet. The World Health Organization estimates that at least 36.9 million people worldwide are infected with HIV/AIDS and that an additional 1.8 million individuals become newly infected each year, approximately 5,000 new cases per day.
Timothy Ray Brown, initially known as the “Berlin patient,” was considered the first HIV-infected patient to be cured. Brown had acquired HIV in 1995 while attending university in Berlin. For 10 years he remained well on antiviral medications that kept the infection in check. In 2005 he developed acute myeloid leukemia, a cancer of the blood cells that develops in the marrow of the bones. This leads to symptoms such as shortness of breath and fatigue and can be rapidly fatal without treatment.
 Timothy Ray Brown, the “Berlin Patient.” Credit: Manuel Valdes, AP
Timothy Ray Brown, the “Berlin Patient.” Credit: Manuel Valdes, AP
Initially, he underwent chemotherapy, which put the cancer into remission. As a precaution, Brown’s oncologist obtained a blood sample to test for a possible stem cell transplant as a next option in case the remission was of short duration. Most patients won’t find a donor match, but fortuitously for Brown, he had 267 matches, which led his doctors to consider finding a donor with recently identified mutations in their white blood cells that make them resistant to HIV infection. (This inherited mutation is called CCR5 delta 32 and is discussed below.)
When the leukemia rebounded in late 2006, Brown decided to go ahead with the transplant. Such medical procedures are, however, complex and carry significant and potentially lethal complications. They are generally only used after more conventional treatments for cancer have already failed. He stopped his antiviral medications, and within three months the HIV was no longer found in his bloodstream.
In Brown’s case, his leukemia recurred a year later, and he underwent a second transfer with the same donor. Complications with the second procedure included severe brain injury that left him nearly blind and paralyzed with a prolonged but eventually full recovery.
As a result of the two bone marrow transplants, however, Brown has since remained free of HIV.
The white blood cells searched for by Brown’s doctors are those with a mutation to their CCR5 receptor on CD4+ T-cells. These cells, helper T-cells that express the CD4 protein on their surface, assist other white blood cells by regulating immune responses to an assortment of infections or pathogens. Helper T-cells are infected by HIV when the virus uses a combination of the CCR5 protein and the CD4 receptor to infiltrate the cell, in turn disrupting the coordinated functioning of the immune system.
When the number of infected CD4+ T-cells are sufficiently suppressed, this leads to the symptomatic stage of the infection, making the patient susceptible to a host of opportunistic infections popularly known as AIDS. An untreated person with AIDS can die from a common cold in a matter of days, much less from more virulent infections.
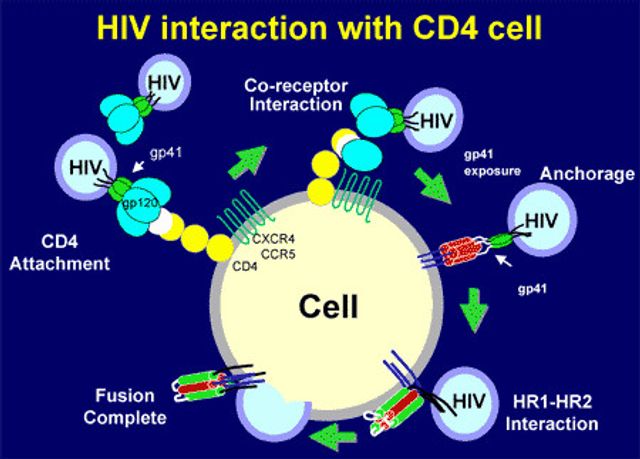 Schematic of how HIV infiltrates a helper T cell using the CCR5 protein and CD4 receptor. Credit: Medscape
Schematic of how HIV infiltrates a helper T cell using the CCR5 protein and CD4 receptor. Credit: Medscape
Proof of individuals resistant to HIV emerged in 1994 when Stephen Crohn was found to be free of the virus after multiple sexual encounters with partners infected with HIV. He was found after several years of research seeking to understand the molecular mechanisms that lead to viral entry into white blood cells. When investigators analyzed Crohn’s blood, they found a mutation that makes a malfunctioning CCR5 receptor, preventing the HIV virus from entering helper T cells.
Since the identification of this mechanism, considerable research has gone into developing therapeutic interventions to block the function of CCR5. Though several drugs called CCR5 receptor antagonists have been studied, Maraviroc, developed by Pfizer and approved by the FDA in August of 2007, remains the first and only CCR5 inhibitor on the market. The drug was found to achieve complete suppression of the virus in 60 percent of people who have had significant resistance to other HIV drugs, though potential serious liver toxicity requires close monitoring.
Advances in HIV treatments, however, have not made access to the drugs for those infected universal. Only 59 percent of people living with HIV are receiving antiviral treatment, leaving 15.2 million human beings constantly in fear of dying from a minor infection.
Moreover, stem cell transplants from CCR5 mutation donors are unlikely to be realistic treatment options for millions affected by the virus. Combination treatment regimens are available, and the transplants carry significant harsh side effects, including the risk of death.
However, having elucidated the molecular pathways and applying the proof of concepts in the treatment of these individuals provides a tremendous impetus towards designing new cures and targeting the treatment for eradicating HIV and possibly future diseases. This will require a global collaborative effort, unfettered by the capitalist market and profit considerations, to coordinate and translate these findings into measurable outcomes.
No comments:
Post a Comment