Kate Randall
A new report reveals that most US states are losing ground on key measures related to life expectancy, which has declined in each of the last three years. The Commonwealth Fund’s “2019 Scorecard on State Health System Performance” shows that “deaths of despair”—premature deaths from suicide, alcohol abuse and drug overdoses—continue to rise in nearly every state. The report further shows that these deaths are tied to rising healthcare costs that are placing an increasing financial burden on families across the country.
The Commonwealth Fund’s Scorecard assessed “deaths of despair” in all 50 states and the District of Columbia, as well as ranked states on 47 measures of access to health care, quality of care, health care usage, health outcomes and income-based health care disparities. The report found that Medicaid expansion under the Affordable Care Act has been a central factor leading to meaningful gains in access to health care.
The reasons behind the decision of a person to take his or her own life, to take drugs resulting in a fatal overdose, or to drink alcohol in excess leading to health problems and death, are complex. But this new study shows that one of the major underlying causes of such tragedies is social inequality, in particular lack of access to health care and the associated financial struggles.
The opioid crisis, suicide and alcohol-related deaths
While the study finds that deaths from suicide and alcohol and drug abuse are a national crisis, it notes that states and regions are affected in different ways. Opioid use disorder has fueled a rise in drug overdose deaths with tragic outcomes for families across the country. The emergence of highly lethal synthetic opioids, such as fentanyl, in the illicit drug supply has contributed to this national crisis.
The opioid epidemic has hit states in New England, the Mid-Atlantic and several Southeastern states particularly hard. West Virginia, Ohio, Pennsylvania, the District of Columbia, Kentucky, Delaware and New Hampshire have the highest death rates from drug overdoses.
In Pennsylvania, Maryland and Ohio, death rates from drug overdose were at least five times higher than from alcohol abuse and about three times higher than suicide rates. In Montana, Nebraska, the Dakotas, Oregon and Wyoming, death rates from suicide and alcohol were greater than those from drugs.
 Source: Commonwealth Fund. Data from National Vital Statistics System
Source: Commonwealth Fund. Data from National Vital Statistics System
West Virginia has been the state hardest hit by the opioid crisis, with 58.7 deaths per 100,000 residents—a staggering two-and-a-half times the national average. This was 25 percent more than the state with the next highest rate of opioid deaths, Ohio, which had 46.3 deaths per 100,000 residents. Opioid-related deaths in West Virginia increased fivefold in 12 years—rising from 10.5 deaths per 100,000 in 2005 to 57.8 in 2017.
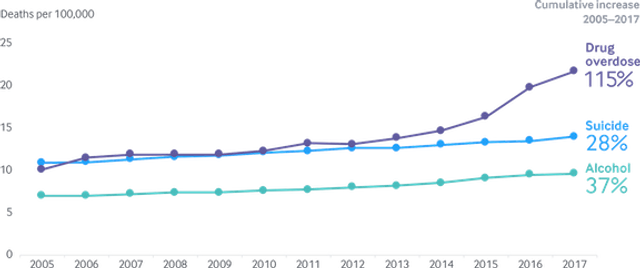
The rate of death from drug overdose more than doubled across the US between 2005 and 2017. These deaths surged by 10 percent just between 2016 and 2017.
Suicide rates nationally have risen by nearly 30 percent since 2005. Parallel to the sharp rise in the death rate from drug overdose, the national suicide death rate rose more sharply between 2016 and 2017 than during any other one-year period in recent history. Similarly, the alcohol-related death rate rose by about 2 percent per year between 2005 and 2012 but increased by about 4 percent per year between 2013 and 2017.
Health insurance, access to care, cost
The Commonwealth Fund notes that the reductions in the uninsured population following the Affordable Care Act’s (ACA) expansion of health coverage in 2014 have now stalled or even begun to erode in some states.
The ACA, commonly known as Obamacare, while expanding some access to health care coverage, has never challenged the domination of the for-profit health care industry. It required that individuals without insurance from their employer or a government program purchase insurance from a private insurance company.
Nearly all states saw substantial reductions in uninsured rates between 2013 and 2017 with the opening of the ACA’s insurance marketplaces, with fewer people citing cost as a barrier to receiving health care.
As the ACA was written, Medicaid, the health insurance program for the poor jointly administered by the federal government and the states, was to be expanded to cover all US citizens and legal residents with incomes up to 133 percent of the poverty line. However, the US Supreme Court ruled in 2012 that it was up to the states whether or not to expand their Medicaid programs.
Almost all those states that expanded Medicaid under the ACA saw a reduction in rates of uninsured through 2015. However, after 2015 any progress in reducing the rates of uninsured had stalled in most states. From 2016 to 2017, more than half of states were simply treading water. Sixteen states saw a rise of 1 percent in the uninsured rate, including both those that did and did not expand Medicaid.
States that adopted Medicaid expansion have seen lower rates of the uninsured. As of January 1, 2017, Massachusetts had the lowest rate of uninsured, at 4 percent. The states with the highest rates of uninsured—Mississippi, Florida, Georgia, Oklahoma and Texas—were among the 19 states that had not expanded Medicaid as of January 1, 2017. In Texas, 24 percent—nearly a quarter of all residents—were uninsured.
Uninsured rates were particularly high in states with large African-American and Hispanic populations. In Florida, George and Texas, about 20 percent of black adults were uninsured in 2017, compared to the US average of about 14 percent. In Texas, more than a third of Hispanic adults were uninsured in 2017. Undoubtedly contributing to the uninsured among Hispanics is the denial of Medicaid and access to the ACA marketplace for undocumented immigrants.
Health care costs
In addition to the lack of health insurance, the high cost of coverage for those who are insured is contributing to the crisis in accessing health care. The report notes that as of the end of 2018, 30 million adults remained uninsured and an estimated 44 million people had insurance but were considered “underinsured” due to the high out-of-pocket costs for health care in relation to their income.
People with individual-market plans under the ACA were insured at the highest rates. However, the cost of private, employer-sponsored health care plans is rising, exposing workers and their families to increasingly higher deductibles and out-of-pocket costs. In most states, the amount that employees contribute to their employer coverage is rising faster than median income.
A key contributing factor to the uninsured and underinsured rates is the overall rate of growth in US health care costs compared to the slow growth in US median income. Workers face rising costs as insurers increase deductibles and other cost-sharing for enrollees. As workers in both ACA and employee plans are covered by the insurance industry, these private companies raise costs for the insured to boost their bottom lines.
The Commonwealth Fund’s report explodes the myth that people’s use of health care services is the primary driver of cost and premium growth. The report notes that there is growing evidence that the prices paid by private insurers to health care providers, particularly hospitals, are responsible for this growth.
The report notes, according to the Health Care Cost Institute, that “between 2013 and 2017 prices for inpatient services paid by private insurers climbed by 16 percent while utilization fell by 5 percent. The analysis found similar patterns for outpatient and professional services as well as prescription drugs.”
In other words, while workers and their families are struggling to obtain decent health care and to pay for it, the entire system of health care delivery in America is geared toward enriching the hospitals, pharmaceuticals and insurance companies. Those succumbing to “deaths of despair” are the victims of a health care system and a society that values capitalist profit over the health and very lives of its citizens.
No comments:
Post a Comment