Benjamin Mateus
On Monday, Severin Schwan, CEO of Swiss diagnostics company Roche, told CNBC’s “Squawk Box” that the United States’ ability to conduct tests to detect the virus that causes COVID-19 infections continues to remain constrained. This comes despite repeated promises by the White House that these tests, numbering in the millions, would soon be available across the nation.
“No doubt, ideally, we would have broader testing,” Schwan said. “But at the moment, capacities are limited. I think this is still a couple of weeks, if not months, out and the reason is very simple.” Schwan said that in the past week, Roche had distributed almost 400,000 test kits across the country.
However, because the virus is spreading so quickly throughout communities, companies are currently not able to manufacture them quickly enough. “The industry is increasing capacities, but at the same time, infection rates are even increasing faster. At the moment, capacities are limited. That is why we have to prioritize testing to higher-risk patients.”
 A person is taken on a stretcher into the United Memorial Medical Center in Houston, Texas after going through testing for COVID-19 on Thursday (AP Photo/David J. Phillip)
A person is taken on a stretcher into the United Memorial Medical Center in Houston, Texas after going through testing for COVID-19 on Thursday (AP Photo/David J. Phillip)
For several weeks running, the World Health Organization has been emphatically counseling all nations to test every suspected case. “If they test positive, isolate them and find out who they have been in contact with two days before they develop symptoms and test those people, too.” The testing is critical to determine not only who is infected but where the virus is spreading. These vital data allow epidemiologists and public health officials to allocate resources to areas becoming affected and stop the transmission of the infection deeper into communities.
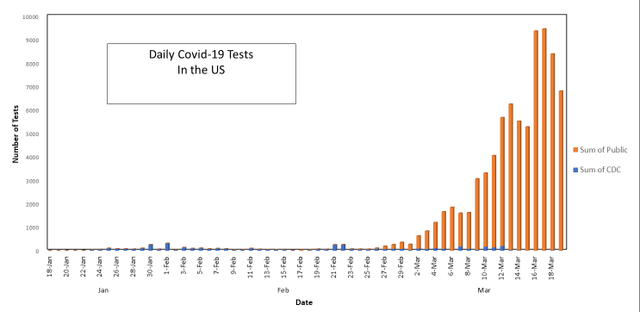
However, due to the disastrous efforts by the US Centers for Disease Control (CDC) to roll out their test kits to states and local labs, the US has been flying blind through the outbreak since the beginning and up to the present moment, in which the epicenter for the pandemic is shifting to the US and now seeing daily new cases approaching 10,000. Health care workers and the public, in general, are vexed by the constant lying by the Trump administration and the assortment of flunkies that attempt to downplay the deadly seriousness of this disease.
As of March 14, testing at the CDC confirming results was no longer required. On its web page, the following statement was posted: “public health laboratories using the CDC assay are no longer required by FDA [Food and Drug Administration] to submit samples to CDC for confirmation. CDC is maintaining surge capacity while focusing on other support to state public health and on improving options for diagnostics for use in the public health sector.” The CDC has relinquished virtually all responsibility to the private sector.
As of March 19, 2020, 83,391 tests had been completed by public health laboratories while the CDC had run 4,651 tests. Although the CDC offers the caveat that clinicians should use their judgment to determine if a patient with signs and symptoms compatible with COVID-19 should be tested—i.e., have fevers, symptoms of respiratory illness like cough or shortness of breath—lack of nasal swabs and test kits preclude a more robust assessment of the population.
The CDC continues to recommend prioritizing testing to hospitalized patients with signs or symptoms of COVID-19 infection, older adults with chronic medical conditions who are at high risk for severe manifestations of COVID-19, or any person, including health care workers, who within 14 days of developing symptoms have had contacts with a known suspect or laboratory-confirmed COVID-19 patient, including those who have traveled from high-risk geographic areas.
 Credit: WSWS
Credit: WSWS
According to the COVID Tracking Project website, US capacity for testing has been accelerating this week, with more than 35,000 tests conducted daily for a total of 359,161 tests to date. A quarter of all these tests were done in New York state, which is facing a disastrous crisis as they are quickly becoming inundated by the rapid growth of new cases.
Dr. Deborah Birx, the White House coronavirus response coordinator, continues to endorse the president’s egregious remarks about “the cure being worse than the disease.” On Tuesday, she said, “there is a fine line and a place to go that balances the needs of the American people both today and tomorrow with the reality of the epidemic.” As a medical professional, her reactionary remarks undermine the warnings made by many distinguished public health experts, epidemiologists and infectious disease specialists that this is a historic pandemic with dangerous consequences.
According to the Washington Post, “epidemiologists and other leading scientists seeking to decipher test result patterns and slow the advance of the coronavirus are stumbling over the huge disparities among the way states administer or report information.”
Caught in the bureaucratic turmoil of the public-private initiative, how test results are reported, how states and private companies share data, if at all, and how states restrict testing create a near-impossible dilemma. According to Dr. Harlan Krumholz, a cardiologist of the Yale School of Medicine and an expert on analyzing the outcomes of a broad range of medical treatments, “We have no systematic strategy to do the kind of surveillance necessary to understand the chain of transmission.” Health officials believe that the number of actual cases throughout the US is considerably higher than what is reported and are concerned that, with time being of the essence, the ability to halt the advance of the contagion will become futile if they are unable to perform mass testing.
Exacerbating this fiasco, as tests have become available, hospitals and drive-through test stations are finding themselves in a bottleneck because they lack enough special nasopharyngeal swabs. Additionally, laboratory directors are also facing a severe shortage of special reagents that can extract the virus’s RNA off these swabs. Clinicians are turning to improvisational methods to obtain these tests, which confound the reliability of negative results.
Dr. Marc Lipsitch, professor of epidemiology at the Harvard School of Public Health, said so succinctly, “The lack of testing in the United States is a debacle. We’re supposed to be the best biomedical powerhouse in the world, and we’re unable to do something almost every other country is doing on an orders-of-magnitude bigger scale.”
No comments:
Post a Comment