Benjamin Mateus
On Monday, the Centers for Disease Control and Prevention (CDC) modified its guidelines for testing for COVID-19. Previously, the CDC recommended that people exposed to close contacts of confirmed cases be tested “because of the potential for asymptomatic and pre-symptomatic transmission.”
This recommendation was changed this week to “if you have been in close contact of a person with a COVID-19 infection for at least 15 minutes but do not have symptoms, you do not necessarily need a test unless you are a vulnerable individual or your health care provider or state or local public health officials recommend you take one.”
 COVID-19 testing of a young girl (Image Credit: Stock Image/Envato)
COVID-19 testing of a young girl (Image Credit: Stock Image/Envato)
The change in guidelines has been met with a barrage of anger and dismay among various health experts and physician groups who have repeatedly stated that the key to suppressing the infection is broad, mass testing of the population.
Former Baltimore Health Commissioner, Dr. Leana Wen, told CNN, “I’m concerned that these recommendations suggest someone who has had substantial exposure to a person with COVID-19 now doesn’t need to get tested. This is key to contact tracing, especially given that up to 50 percent of all transmission is due to people who do not have symptoms. One wonders why these guidelines were changed—is it to justify continued deficit in testing?”
According to sources speaking to the New York Times and CNN, the order came from the Trump administration during a closed meeting without the presence of Dr. Fauci. The CDC has remained silent on providing any explanation on its sudden policy change and directed all questions to the Department of Health and Human Services (HHS).
HHS Assistant Secretary Admiral Brett Giroir released a callous and nonsensical statement that said, “This guidance has been updated to reflect current evidence and best public health practices and to further emphasize using CDC-approved prevention strategies to protect yourself, your family, and the most vulnerable, of all ages.”
Speaking later to CNN, Giroir added that the guidelines were authored by Dr. Fauci, White House coronavirus response coordinator Dr. Deborah Birx, and Stephen Hahn, head of the Food and Drug Administration.
However, Fauci, who was in surgery during the meeting where the changes were approved, told the media, “I am concerned about the interpretation of these recommendations and worried it will give people the incorrect assumption that asymptomatic spread is not of great concern.”
Clearly, the change in guidance is no minor slip and follows President Trump’s repeated assertion that too much testing has been driving the number of cases up in the country. Behind this maneuver is an effort to ensure the public health guidelines conform to demands by Democratic and Republican officials alike for the reopening of schools and continuation of in-person classes.
Recent debacles in attempting to open schools had seen roughly 2,500 teachers, students and staff tested positive for COVID-19 earlier in the month. Now, almost every state in the country has had at least one school report of a COVID-19 outbreak.
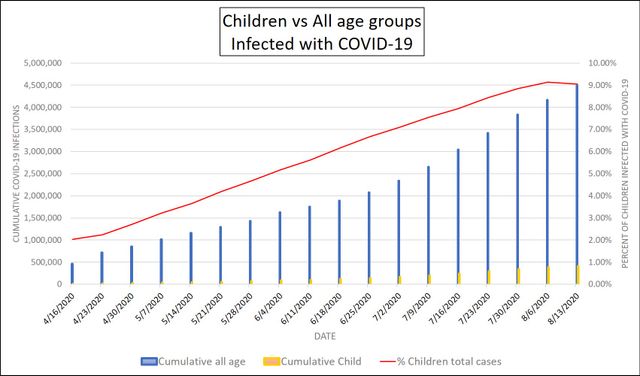 American Academy of Pediatricians—Children vs. all age groups with COVID-19
American Academy of Pediatricians—Children vs. all age groups with COVID-19
CNN reported yesterday that in Mississippi, with a positivity rate where at least one in four tests came back positive for COVID-19, nearly 4,000 students and almost 600 teachers have quarantined due to exposure. In Florida, where Governor Ron DeSantis has likened school reopening to the Navy SEALs mission to assassinate Osama bin Laden, almost 9,000 children have been diagnosed over the last two weeks. Reports also indicate that the number of children hospitalized has risen 38 percent over the same period to 602 in the most recent announcement.
The social anger and resentment among teachers, parents, and students is palpable and growing. Lack of preparation, utter ineptitude on the part of school officials and teachers unions, and significant pressure being brought to bear from every level of the state are forcing every community to face the significant dangers associated with COVID-19.
Just in the last two weeks, more than 74,000 children in the US tested positive for the coronavirus, a 21 percent increase between August 6 to August 20. According to the American Academy of Pediatrics, presently, there have been at least 442,785 confirmed cases of COVID-19 in this age group. Since May, when states proceeded out of lockdowns and opened commerce, children have been a growing section of COVID-19 cases. They presently account for nearly 10 percent of all cases of COVID-19 in the country.
The new testing guidelines fly in the face of earlier studies by the CDC which established that children are more likely to be asymptomatic carriers of the infection but can spread the disease as well as adults. Studies from Italy, South Korea and the US have confirmed that children carry the same or higher viral loads in their nasal sinuses as adults. Documented reports in camps and schools have demonstrated that children are excellent vectors for the transmission of the coronavirus.
The percent of the population that is asymptomatic or pre-symptomatic is still an open question for epidemiologists. The Washington Post published on August 8 a summary of studies in various specific communities which found a wide range in the share of asymptomatic infections. The most often cited reference presently comes from the CDC that places the figure at 40 percent. A small study from South Korea further characterized that only approximately 20 percent of asymptomatic patients will go on to develop symptoms over a median interval of 15 days.
Besides being a significant factor and challenge in the high rate of community transmission, the long-term complications associated with COVID-19—which need urgent study—include lung, heart and kidney injury that could develop into chronic health problems.
Regardless of the decreased propensity of morbidity and death from COVID-19 among children and young adults, this group constitutes close to 95 million people representing almost 30 percent of the country. A death toll of 1 in a 1,000 would mean tens-of-thousands of deaths in these age ranges that could have been prevented. According to the American Academy of Pediatrics, mortality among children in 45 states and New York City has ranged from 0 to 0.7 percent.
Equally concerning, teachers at high risk for severe COVID-19 infections account for 1 in 4 educators or 1.5 million people. Additionally, millions of elderly people live in homes with school-aged children. The Trump administration’s push to suppress testing will be catastrophic.
Despite the decline from the July days that saw daily cases reach above 70,000, the present transmission rate remains excessive, with over 40,000 new confirmed each day, and 1,000 people are dying each day. The United States will pass 6 million cases this week and is poised to exceed 200,000 deaths in the first half of September.
Even as the White House moves to suppress testing, health officials are seeing new COVID-19 cases across rural areas of the “heartland” states which had not been as hard hit as the rest of the country. Kansas Governor Laura Kelly reported that there had been a case of COVID-19 in every county in the state, and the seven day-average in cases has been steadily creeping upwards. Last week, the University of Kansas reported over 80 COVID-19 infections on campus.
The Wall Street Journal reported on Monday that eight of ten counties in Illinois that have had the fastest rates of new COVID-19 cases per capita have been in rural districts, a reversal of trends when Cook County, the home of Chicago, dominated cases early in the course of the pandemic.
The latest outbreaks in Illinois have been directly attributed to the return of students to K-12 schools and universities, which is potentially a harbinger of growing community transmission as cold weather will begin to push people indoors in the next two to three months. The University of Illinois Urbana-Champaign is expecting to see more than 200 students with COVID-19 infections among the returning 40,000 students.
Governor of Ohio Mike DeWine reported that the counties of Drake, Mercer and Jackson had recorded the highest new COVID-19 cases per 100,000 residents. The state has allowed outdoor and indoor sports venues to operate under supposed restrictions of 15 percent of seating capacity. With over 4,000 confirmed deaths in the state, Governor DeWine, defending his handling of the pandemic, told the local press, “…the long-term gain is not just we’ve saved lives. The long-term gain is we don’t destroy our economy.”
Compounding the United States’ testing woes, a recent report by Tori Marsh from GoodRx reported that 67 million Americans in both metropolitan and rural communities are on average over 22 miles from the nearest COVID-19 testing center. Texas, California, Florida, Ohio and Michigan have some of the largest numbers of COVID-19 testing deserts, defined as a census tract that is at least 10 miles away from a testing center. The median income for census tracts in testing deserts is $52,462 compared to $67,964 for non-desert census tracts.