Benjamin Mateus
The Centers for Disease Control and Prevention (CDC) released a press brief Monday noting that the number of fatalities currently attributed to COVID-19 make it the third leading cause of death in the United States this year, behind heart disease and cancer.
The Worldometer’s COVID-19 tracker places the number of confirmed cases in the United States over 5.6 million, with 175,000 deaths as of this writing and the toll continues to rise by more than 1,000 every day. The Institute for Health Metrics and Evaluation (IHME) at the University of Washington currently forecasts that over 251,000 Americans will have lost their lives to COVID-19 by November 1 if current projections hold.
According to the CDC, the ten leading causes of death for the non-pandemic year 2018 in descending order were heart disease (647,457), cancer (599,108), accidents/unintentional injuries, (169,936), chronic lower respiratory disease (160,201), stroke (146,383) Alzheimer disease (121,404), diabetes (83,564), Influenza and pneumonia (55,672), kidney disease (50,633) and suicide (47,173).
The first official COVID-19 death occurred on February 28 in Seattle, Washington, a man in his 50s who had underlying health conditions. However, postmortem testing on deaths from Santa Clara County suggests the first deaths took place earlier in the month.
 Patient in an Intensive Care Unit
Patient in an Intensive Care Unit
The sole fact that COVID-19 deaths have become the third leading (preventable) cause of death in the US speaks to the utter negligence and criminality on the part of the Trump administration and the ruling class. Had lockdown been initiated earnestly two weeks earlier than was the case in March, epidemiologists estimate 54,000 fewer people would have died by early May when the official death toll surpassed 70,000.
Ali Mokdad, a professor of Global Health at the IHME, speaking to Healthline about the US death toll fast approaching a quarter million people, said, “Unfortunately, that is the track we’re on. We have pretty much totally relaxed some of our social distancing mandates because there is a big concern about the economy…These are not just numbers. These are loved ones, family members, essential workers who sustain our economy.”
The latest predictions have not taken into account excess mortality figures, which the New York Times found show that at least 200,000 more people have died than usual since March, 60,000 higher than the number of deaths that have been directly linked to COVID-19.
To place the toll of the current pandemic into its proper historical context, it would be worthy to briefly review a recent study that compared its impact so far to the devastating Spanish flu which stuck the globe a little over 100 years ago.
 Nurse from 1918 with guidance to the public (Credit: Photo by Everett/Shutterstock)
Nurse from 1918 with guidance to the public (Credit: Photo by Everett/Shutterstock)
The 1918 H1N1 influenza pandemic killed 675,000 people in the United States. In a comparative study recently published in JAMA Network, during the peak of the 1918 pandemic in New York City (NYC), 31,589 all-cause deaths occurred among 5,500,000 residents. This yielded a mortality incidence rate of 287 deaths per 100,000 persons-months. This was 2.8 times higher than the preceding four years, which averaged around 100 deaths per 100,000 persons-month.
During the height of the COVID-19 outbreak in NYC in April, 33,465 all-cause deaths occurred among a population of 8,280,000, placing the incidence rate at 202 deaths per 100,000 persons-months. The scale of incident deaths during the COVID-19 pandemic is very much comparable to the health crisis that affected the city a century ago.
However, given the advances in medicine, public health, and safety, the incidence of all-cause mortality in the preceding years was 50 per 100,000 persons-month. In other words, the all-cause mortality compared to the previous years, from 2017 to 2019, is 4.15 times higher. In this light, to equate the present coronavirus pandemic to the seasonal flu is simply malicious.
The opening of the economy in late spring coincided with the ramping up of COVID-19 testing and apparent plateau in infections. What many commentators did not take an adequate measure of was that the number of cases across the country appeared stable because New York state was seeing dramatic declines in their new cases after implementing a massive shutdown of the city. What was happening in the rest of the country was a rapid increase in numbers hidden in the static created by New York’s massive amount of cases.
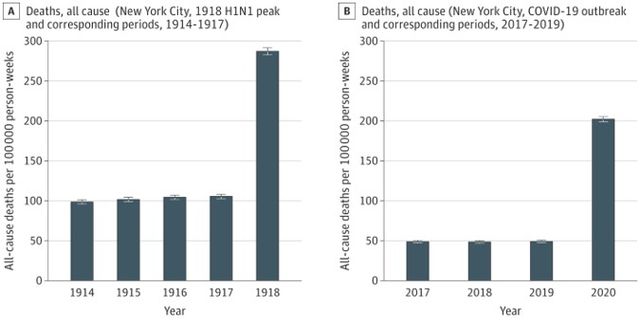 Comparison between Spanish Flu and COVID-19 in NYC
Comparison between Spanish Flu and COVID-19 in NYC
Once New York State’s numbers had plummeted sufficiently, it became evident that the half-hearted measures in the rest of the country had done little to contain the pandemic.
Testing was now clearly revealing that the epidemic had become deeply entrenched along a broad geographic region leading Trump to make his infamous complaint that, with more testing, you get more cases. As cases rose to record heights, death followed with the gruesome scenes witnessed in New York replayed in Florida, Texas, Arizona and elsewhere throughout the country.
As hospitals in these states filled up and morgues pushed to over-capacity, mandates were reinstituted for social distancing and mask wearing. Bars and restaurants were ordered closed by governors who had been utterly resistant to imposing any restrictions as the virus spread into their communities.
However, as schools were preparing to reopen for face-to-face classes in a few weeks, the scope of “more” testing became a point of contention for the White House. In mid-July, in conjunction with the transfer of responsibility on hospitalization reporting from the CDC to the Department of Health and Human Services there was a sudden decline in the number of daily testing across the country, predominately in the hardest-hit states. Not surprisingly, the decrease in the number of new cases quickly followed as reports were appearing that the virus was spreading in states like Georgia, Mississippi, Tennessee, Missouri, and Iowa.
Yesterday, the New York Times reported that there had been only 40,022 new cases confirmed on Monday, with only 542 deaths. The weekly average had dropped 16 percent from two weeks before to 50,543 cases per day. Over the same intervening period, the seven-day average for tests per day had fallen 10 percent to 736,000.
Sadiya Khan, assistant professor of cardiology and preventive medicine at Northwestern University’s Feinberg School of Medicine, told U . S . News & World Report, “I want to be enthusiastic about the numbers going down, but it’s really hard to convince me that it’s not because we’re just doing fewer tests. The dramatic drop is very concerning while we see schools reopening, businesses reopening, and we’re trying to move our economy forward, and yet we’re not prepared.” On Tuesday, the US conducted 642,814 tests, according to the Covid Tracking Project, well below the already falling average.
The blame has been cast on a lack of capacity for such a large number of testing caused by a shortage of supplies, trained personnel, and machines that can perform mass throughput analysis, which has led to delays in reporting numbers. The nature of decentralized private labs without a coordinated national supply chain has been cited as the main factor. Several media outlets have noted that the number of people going to testing sites has been declining out of apathy and frustrations with long delays in reporting. A survey conducted by CNBC found almost 40 percent of Americans had to wait more than three days for their results, which makes the results useless as the window for contact tracing is 48 hours or less.
According to TIME, the Federal Emergency Management Agency (FEMA) is supposedly working with states in an attempt to resolve these bottlenecks. National stockpiles are empty, and so FEMA competes with labs for the same supplies. They write, “FEMA sends supplies it receives to the states, which then send them to the labs. But health policy experts and lab directors interviewed by TIME say it’s unclear how many supplies FEMA is procuring and how the states are distributing them.”
Adding to the confusion, major case reporting errors have further exacerbated accurate counting. The Associated Press reported that in Iowa, “potentially thousands of coronavirus infections from recent weeks and months have instead been erroneously recorded as having happened in March, April, May, and June.” Last week the California Department of Health and Human Services Secretary reported that a server outage led to delays in reporting results from a backlog of 250,000 to 300,000 tests.
With declining testing, there is a correlation with rising test positivity. Johns Hopkins coronavirus resource center has noted percent positivity rate for recently hard-hit states—Nevada 17.1, Idaho 16.6, Florida 16.4, Mississippi 15.9, Texas, 13.0, Kansas, 12.5, Georgia 12.0, Iowa 11.2, Missouri 9.8, Indiana 9.6, Nebraska 9.5 and Arizona 9.2—have been climbing. Only 19 states have positivity rates under 5 percent, the lax criteria set by the World Health Organization for reopening schools. The CDC also noted that percent positive tests for ages 0 to 4 and 5 to 17 years old exceed ten percent and are climbing.
The ruling class, for its purposes, has learned it is best to fly blind through the pandemic.
No comments:
Post a Comment